What Doctors Don't Know, But Should
Oct 13, 2016 08:15
The practice of medicine has changed considerably over the last couple of decades. In the past, medicine was based on the Aristotelian method. Physicians were instructed to understand the disease before they prescribed any treatment.
In principle, it sounded like a good idea. If you could know what was going wrong in a condition, you could then design a treatment to resolve it. At the dawn of modern medicine, this worked awfully well. Frederick Banting and Charles Best realised that diabetes was caused by a lack of insulin in the body following experiments on dogs. Therefore, they set about making their own insulin to inject into human patients. If their understanding of the disease was correct, giving diabetic insulin should resolve the problem. They were right, of course. And now both men are celebrated in the annals of medical history.
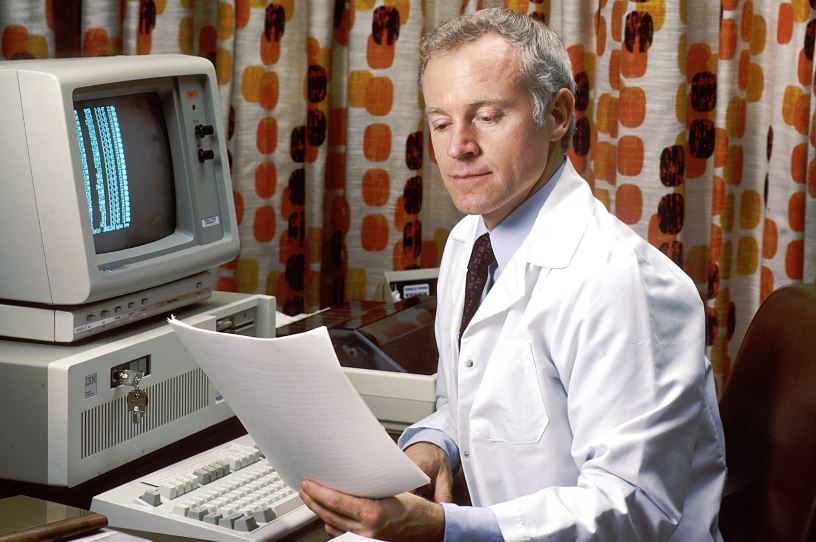
Wikimedia Commons
But there have been times when the Aristotelian method has come up short. Just take the whole fiasco involving HRT therapy. Doctors believed that the treatment would take the edge of menopause symptoms and help women live longer. They reasoned like Banting and Best had with diabetes, that the problem was a lack of estrogen. So they replaced it with their own synthesised hormones, thinking it would work. It didn’t. And ultimately it wound up increasing women’s risk of breast cancer sixfold.
Modern medicine is in something of an upheaval right now. The old mantra that we need to stick to understanding diseases first and move to treatment later is going away. And with it, so are the way that doctors are being perceived.
Consider this. Practically every other profession is evidence-based. If something doesn’t work, it doesn’t matter if the theory says it should. The data are what counts. In finance for example, if a stock keeps losing money, an investor won’t continue to invest in it. They’ll look for an opportunity somewhere else where the returns are more favorable. Or what about an educator? Educators don’t just keep trying the same methods of teaching over and over until a method works. Instead, they home in on a strategy that has the most impact among their students.
In many ways, doctors are the final authority in our society to crumble to the supremacy of data. Doctors will often prescribe drugs, based on their “understanding” of a disease, even if the drugs don’t work. In fact, there are still many doctors today who will write off evidence because of their love of the theory. Take the HERS study, for instance. Here it was shown that taking estrogen didn’t have any effect on the rate of heart disease. And yet doctors still continued to refuse to believe it.
It should be noted that physicians are starting to get their acts together. More and more are attending influenza knowledge transfer series and other continuing medical education. And they’re also getting to grips with the latest in lifestyle medicine, which is a significant change from the past.
But there’s a long way to go of course. And the influence of drug companies in both training and practice remains extensive. But the move towards evidence-based medicine should at least provide the foundation for more rigour in treatment.
In principle, it sounded like a good idea. If you could know what was going wrong in a condition, you could then design a treatment to resolve it. At the dawn of modern medicine, this worked awfully well. Frederick Banting and Charles Best realised that diabetes was caused by a lack of insulin in the body following experiments on dogs. Therefore, they set about making their own insulin to inject into human patients. If their understanding of the disease was correct, giving diabetic insulin should resolve the problem. They were right, of course. And now both men are celebrated in the annals of medical history.
Wikimedia Commons
But there have been times when the Aristotelian method has come up short. Just take the whole fiasco involving HRT therapy. Doctors believed that the treatment would take the edge of menopause symptoms and help women live longer. They reasoned like Banting and Best had with diabetes, that the problem was a lack of estrogen. So they replaced it with their own synthesised hormones, thinking it would work. It didn’t. And ultimately it wound up increasing women’s risk of breast cancer sixfold.
Modern medicine is in something of an upheaval right now. The old mantra that we need to stick to understanding diseases first and move to treatment later is going away. And with it, so are the way that doctors are being perceived.
Consider this. Practically every other profession is evidence-based. If something doesn’t work, it doesn’t matter if the theory says it should. The data are what counts. In finance for example, if a stock keeps losing money, an investor won’t continue to invest in it. They’ll look for an opportunity somewhere else where the returns are more favorable. Or what about an educator? Educators don’t just keep trying the same methods of teaching over and over until a method works. Instead, they home in on a strategy that has the most impact among their students.
In many ways, doctors are the final authority in our society to crumble to the supremacy of data. Doctors will often prescribe drugs, based on their “understanding” of a disease, even if the drugs don’t work. In fact, there are still many doctors today who will write off evidence because of their love of the theory. Take the HERS study, for instance. Here it was shown that taking estrogen didn’t have any effect on the rate of heart disease. And yet doctors still continued to refuse to believe it.
It should be noted that physicians are starting to get their acts together. More and more are attending influenza knowledge transfer series and other continuing medical education. And they’re also getting to grips with the latest in lifestyle medicine, which is a significant change from the past.
But there’s a long way to go of course. And the influence of drug companies in both training and practice remains extensive. But the move towards evidence-based medicine should at least provide the foundation for more rigour in treatment.