Nurse practitioners and technology: Examining the impact
Dec 14, 2023 01:16
Technology has transformed many industries, including healthcare. The changes that the healthcare space has undergone in recent decades are largely for the better. Several different technological advancements have positively impacted the workday for nurse practitioners. These improvements include electronic health records (EHRs), telemedicine, mobile health apps, and virtual assistant technologies.

In addition to improving the workday for nurse practitioners, technology in healthcare improves patient experiences, reduces costs, and allows for more efficient healthcare delivery. Telemedicine makes it easier for nurse practitioners to reach patients who live in rural areas. Electronic health records allow nurse practitioners to access patient records in a much more efficient way.
Both of these use cases are discussed below, but ultimately, the outcome is that technology helps the nurse practitioner more easily navigate their daily responsibilities. As a result, patients benefit.
The difference full practice authority makes
In Kansas, a nurse practitioner’s full career practice authority allows nurse practitioners to see patients without needing to consult with a physician. Rockhurst University has a range of online nursing programs that prepare students from all levels of nursing with the advanced skills and evidence-based practices needed for a rewarding career in nursing. The nurse practitioners can prescribe medications, as well as order lab tests, imaging studies, and other diagnostic tests. Essentially, they can provide the same type of care that one would otherwise receive from a family physician.
Additionally, full practice authority helps to fill the growing gap for primary care services. The population is aging, and there are not enough primary care physicians to meet demand. Caregiver burnout also contributes to a shortage of qualified healthcare professionals.
Exploring electronic health records
Electronic health records represent one major advancement that enables many benefits to healthcare professionals, particularly nurse practitioners. EHRs make it very easy for nurse practitioners to retrieve the needed patient information and do so quickly and more efficiently than the legacy paper-based medical record systems allow.
EHRs also reduce paperwork. Reduced administrative burdens like this free up the valuable time of nurse practitioners so they can spend more time on direct patient care and really make the most of those interactions.
While EHRs come with their own set of documentation requirements needed to meet regulatory compliance, virtual assistant technologies have been used with success to allow clinicians to take notes during patient encounters by using voice commands. Voice technology enables nurse practitioners to order tests such as an MRI or retrieve notes from the last consultation the patient had.
Using mobile apps for better health outcomes
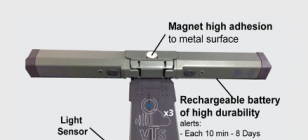
Mobile health apps are very beneficial for helping patients track vital signs and allowing practitioners to both monitor and manage health conditions. Mobile health apps can help lead to better health outcomes. The instant monitoring that health apps can provide is valuable for patients with chronic conditions that need continual monitoring, such as diabetes. Medication tracking features and reminders help app users ensure that they do not miss a dose. This reduced risk of disruption to treatment leads to better outcomes for patients.
Exploring patient portals and integrated care coordination platforms
The patient portals that many hospitals offer allow patients to communicate directly with their nurse practitioner and healthcare team. This helps to ensure the patient is an active participant in their healthcare journey and is kept informed every step of the way.
The ease of accessing records does keep patients engaged. An additional benefit of patient portals is that they promote patient education. Nurse practitioners play an important role in patient education. They explain diagnoses and treatment options to their patients. Informed and educated patients are more likely to comply with treatment plans.
Integrated care coordination platforms help not only nurse practitioners, but all members of a patient’s healthcare team — allowing them to get a comprehensive view of patient data. They offer a way to consolidate an abundance of information in one place. Nurse practitioners can make more informed decisions and more easily coordinate with other members of the healthcare team.
Artificial intelligence and healthcare use cases
Artificial intelligence (AI) can be used for more than just scheduling appointments in healthcare settings. AI-based diagnostic tools assist clinicians with predicting disease progression and even diagnosing cancer before symptoms are present. Komodo Health offers software solutions that use data analytics and machine learning to help diagnose cancer earlier with their Healthcare Map serving as the basis of their solutions. Access to tools like this leads to better treatment outcomes and increases the possibility of remission or cure.
We might still be a long way from where AI can act as a copilot in healthcare settings, but there are currently some remarkable uses of AI, machine learning, and data analytics in healthcare. AI can lead to more data-driven healthcare. It also facilitates more patient-focused care, in part through the personalization that access to data allows.
Health information exchange systems and their benefits
Health information exchange systems (HIEs) allow for sharing of data between separate hospitals or healthcare organizations. When doctors and nurse practitioners in different healthcare organizations have access to the same information at the click of a button, patient care improves. HIEs reduce the likelihood that duplicate tests and procedures will be ordered. This helps to reduce healthcare costs, but it also helps patients get the right care in a timely manner. HIEs break down data silos that exist in isolation. Diagnoses can happen quicker and end up being more accurate.
Prescription management software has enhanced patient care because it reduces medication errors caused by illegible handwriting. It also ensures pharmacists receive accurate instructions. Additionally, prescription management software provides alerts to the nurse practitioner if there are any potential drug interactions with a patient’s existing medications. The software also triggers allergy alerts. These alerts allow the nurse practitioner to make any needed adjustments.
The benefits of telemedicine for nurse practitioners
Telemedicine has also improved the daily workday for nurse practitioners. Telemedicine allows nurse practitioners to assist patients who might otherwise have limited access to healthcare. The NP can assess patients and triage effectively.
The future is promising for the use of technology in healthcare. Technological advancements will likely continue to drive improvements in how care is delivered to patients, and, whilst doing so, it is already offering many benefits to nurse practitioners and patients.