The Intersection Of Technology And Therapy In Addiction Treatment
Jan 08, 2024 15:01

Substance use disorders are complex health conditions that affect millions of Americans each year. According to the 2021 National Survey on Drug Use and Health (NSDUH), almost one in three adults had either a mental illness or suffered from substance use disorder in the previous year.
Treating different types of disorders requires an individualized multifaceted approach, including counseling, support groups, medication, and lifestyle changes.
For many years, technology has emerged as a valuable tool in personalizing and supplementing traditional addiction treatment methods. From smartphone apps to virtual reality simulations, it’s transforming how clinicians and patients approach treatment.
Here’s a comprehensive discussion on how humans and machines work together to address substance use disorders.
Common Addictions Treated In Rehab Centers
Addiction treatment or rehab facilities offer programs providing care, counseling, and support for individuals struggling with a wide range of substances and behavioral addictions. While admission terms vary from center to center, they address a few of the most prevalent addictions, such as the following:
· Alcoholism
This condition describes physiological and psychological dependence on alcohol consumption and remains the most commonly treated addiction globally. For instance, the 2022 NSDUH survey revealed that 29.5 million individuals aged 12 and older were suffering from alcohol use disorder in 2021.
· Cannabis Addiction
Evidence shows that about 21% of patients who use cannabis develop a dependence on it, leading to withdrawal symptoms and life disruption.
• Gambling Disorder
Behavioral and neurological components drive compulsion to risky reward-seeking gambling despite the prospect of negative consequences. About 1% of the American population is suffering from this condition, according to research by Yale Medicine.
· Nicotine Addiction
Tobacco usage accounts for over seven million deaths globally, per the Centers for Disease Control and Prevention (CDC). Despite this, nicotine addiction is among the most difficult substance use disorders to address.
· Opioid Addiction
This substance use disorder refers to excessive use of narcotic pain medications, like oxycodone or heroin, resulting in chemical dependence. The opioid epidemic is a leading public health crisis.
· Stimulant Addiction
Compulsive use of energizing substances—such as cocaine, methamphetamine, or amphetamine (e.g., Adderall)—is the hallmark of stimulant addiction. It’s also one of the more common forms of substance use disorders in the country.
Treatment centers also aid in recovery from sedative addictions involving benzodiazepines, barbiturates, or sleep medications. Rehab facilities may additionally focus on process addictions, such as those related to sex, porn, gaming, social media, or eating disorders. These behavioral addictions stimulate the brain’s reward system in a way substances do.
Overview Of Common Addiction Therapies
Understanding addiction’s many manifestations is key to mitigating its collective societal damage through science-based care. An individual’s treatment plan will depend on multiple factors, including the length and severity of use, the type of addiction, and its impact on the patient.
Most quality addiction treatment programs incorporate these approaches:
· Cognitive Behavioral Therapy
CBT focuses on identifying negative thought patterns that trigger substance abuse and then learning healthier coping strategies and beliefs.
· Motivational Interviewing
This modality seeks to build the patient’s internal motivation for change through empathetic, nonjudgmental counseling.
· Group Counseling
Patients facing similar struggles are brought together to share resources, experiences, and support. Forming peer groups facilitates community, accountability, and learning.
· Medication-Assisted Treatment
Opioid prescription medications—e.g., buprenorphine, methadone, or naltrexone—alleviate withdrawal symptoms, reduce cravings, or block rewarding effects during detox and maintenance.
· Contingency Management
This method encourages positive behaviors by providing rewards for achieving treatment goals or negative drug tests. These may include vouchers, prize draws, or specific privileges.
· 12-Step Programs
Programs like Alcoholics Anonymous and Narcotics Anonymous connect people seeking sobriety through spirituality and a series of self-improvement steps. Meetings provide mentoring and a sober support network.
While apps and digital tools hold exciting potential, treatment centers integrate technology alongside human-led therapies. After all, technology serves as a valuable enhancement, not a replacement for addiction treatment. These therapies utilize human connection and science-backed techniques to target root causes driving substance misuse at the individual level.
How Rehab Centers Use Technology For Therapy
The convergence of technology and therapy promises many benefits for the field of addiction medicine. Combining tech’s versatility and scalability with the empathy, accountability, and wisdom gleaned from counseling fosters better outcomes.
Digital tools can increase access to care for underserved populations, provide continuous support outside the clinic, and offer new ways to understand and modify addictive behaviors.
Understanding traditional modalities forms a foundation for evaluating how emerging innovations can enhance addiction medicine via high-tech and human-touch approaches.
1. Enhancing Pre-Treatment Data Gathering
Technology is being utilized in various ways to help plan appropriate treatment for those with addictive disorders.
· Assessment And Diagnosis
Mobile and online screening tools can help identify potential signs of addiction and connect people to treatment resources. These can increase access to assessment for underserved groups.
· Personalized Treatment Planning
Machine learning and artificial intelligence (AI) integration enable customized treatment plans tailored to individuals’ unique needs. By analyzing patient data and patterns, algorithms can match people to optimal types and levels of care and allow patients to indicate treatment preferences.
· Predicting Outcomes
Looking at population health data, predictive analytics tools can forecast which patients have higher risks of relapse based on attributes like demographics, mental health comorbidities, treatment history, etc. These algorithms help clinicians provide targeted intervention resources.
· Evaluating Treatment Options
Treatment search platforms aggregate information on various facilities’ treatment philosophies, services offered, patient reviews, and outcomes. This can assist clinicians, patients, and their loved ones in evaluating the best fit and conducting virtual tours of facilities as well.
Overall, technology supports a data-driven precision approach to addiction treatment planning by understanding individual patient needs rather than relying on a one-size-fits-all model.
2. Telehealth And Mobile Health Apps
Digital tools can extend the reach of addiction treatment beyond traditional facilities. Telehealth platforms let patients access counseling, medication management, and peer support groups remotely via video chat or phone.
Similarly, mobile health (mHealth) apps create opportunities for 24/7 access to support, information, and tracking from a patient’s smartphone. Relevant apps can assist with sobriety, withdrawal, and relapse prevention through features like peer discussion boards, distracting games and videos, medication reminders, healthy coping recommendations, and journals to log cravings or trigger situations.
Better Care Continuum
The flexibility of telehealth removes transportation barriers and helps accommodate busy schedules, making it easier for patients to engage in regular care. Telehealth and mHealth apps also enable discreet access from home, which may appeal to populations hesitant to visit traditional addiction treatment facilities due to stigma.
Across diverse demographic and socioeconomic groups, utilizing tech as an additional touchpoint for addiction care can supplement face-to-face services to promote better continuity of care. Putting resources directly in the hands of those struggling with addiction, mHealth apps equip patients with tools for managing their health outside of their weekly therapy appointments.
3. AI, Wearables, And Digital Phenotyping
AI-integrated solutions, wearable biosensors, and digital phenotyping tools demonstrate how emerging technology could revolutionize addiction medicine down to the individual level.
· AI solutions
Chatbots and virtual assistants, while still in the early stages, show promise as low-cost counseling and recovery support that scale to serve more people. Some apps use machine learning to provide personalized feedback based on patients’ usage patterns and self-reported data.
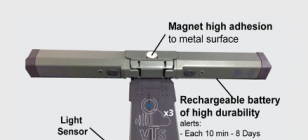
· Biosensors
Wearable devices like watches, rings, or patches can continuously gather physiological data relevant to substance use and cravings, such as heart rate variability and skin temperature. This biosensor data offers clinicians an objective window into patients’ health patterns outside the treatment setting.
Combining patient self-reports with sensor analytics enables more fine-grained diagnostics and treatment adjustments.
· Digital Phenotyping
Digital phenotyping, which uses smartphone functions to gather relevant data, also shows promise for passively gathering data to detect emerging addiction issues sooner. The analytics field of digital phenotyping goes a step further by assessing digital breadcrumbs from patients’ smartphone or Internet activity. This could mean examining communication patterns, mobility data, typing speed, or even social media posts.
Changes in digital behavior may reflect emerging mental health issues or risk of relapse, allowing clinicians to intervene earlier. While still largely an academic research area, digital phenotyping demonstrates how everyday technologies could be utilized to predict and prevent substance use disorders.
Potentials And Limitations
The wealth of health data these tools unlock holds exciting possibilities for gains in treatment efficacy and scientific understanding of addiction. However, the accuracy of AI and analytics relies heavily on access to quality training data across diverse populations.
There also remains much to explore around the clinical validity and reliability of emerging monitoring technologies. As adoption spreads, maintaining rigorous research on the impact of these innovations through clinical trials and long-term studies will be critical.
4. Virtual Reality And Gamification
Technologies like virtual reality (VR) and gamification show promise by employing immersion and motivation for treating the behavioral components of addiction. VR uses simulated scenarios to trigger and modify learned addictive behaviors.
Users confronting simulations of high-risk situations like a party with drugs or a liquor store can practice coping mechanisms to increase self-efficacy. Therapists monitor patients during these VR exposures and lead debriefing discussions to solidify positive learning.
The gaming industry also provides key insights on using motivation, incentives, and duplication to drive habit formation, which researchers are now applying to support addiction recovery. Gamified apps feature point systems, challenges, bonuses, and social elements to incentivize abstinence and adherence to treatment plans. Making recovery competitive and game-like aims to boost engagement, especially among adolescents and young adults already accustomed to quantifying progress through technology use.
Potentials And Limitations
Both VR and gamification speak to the importance of motivation and environment as contributors to addiction. While much of the hype outpaces the clinical research at this stage, interacting with patients through familiar digital mediums could enhance traditional talk therapy’s impact. These tools show particular promise for youth addiction treatment by meeting patients where they are most engaged.
5. Implementing Tech-Assisted Treatment Thoughtfully
As digital solutions slowly make their way into the addiction treatment landscape, realizing the full benefits will require strategic implementation grounded in scientific evidence. While technology enables new modes of access, measurement, and communication, developing responsible use policies will help protect patients.
· Sticking To Individual Treatment Goals
Isolated use of any apps or gadgets without the context of treatment goals and medical knowledge can lead to misinformation or even harm. Integrating tech as part of comprehensive, individualized treatment plans is key.
· Training Patients And Care Staff
Another priority is expanding technical fluency and digital literacy for both addiction medicine clinicians and patients. Clinicians need training to evaluate the clinical credibility of apps, along with competency for interpreting data from digital devices and making data-informed recommendations.
Similarly, patients adopting tech aids would benefit from guidance on assessing quality, avoiding misuse, and setting reasonable expectations regarding privacy. Developing codes of conduct around the ethical use of data and AI will help the field adopt best practices as these tools evolve.
· Measuring Impact
Continuing research on emerging therapies remains crucial as they transition from theoretical to clinical application. While VR, wearables, and similar innovations show immense promise, real-world evidence of successful adoption and efficacy is limited. As consumers and healthcare systems get excited by the hype of technology for addiction treatment, maintaining rigorous research standards will help ensure a lasting positive impact.
· Putting Patients At The Forefront
However, effectively integrating tech into treatment also introduces ethical considerations around patient privacy and the clinical evidence behind new interventions. As the possibilities rapidly unfold, the addiction treatment community must thoughtfully evaluate each innovation through the lens of patient well-being.
Managing public enthusiasm through responsible regulation, clinician training, and ongoing research will help ensure that tech-based treatments complement existing evidence-based approaches. Technology has already begun transforming traditional substance use disorder therapy by opening new possibilities for evaluation, accessibility, and understanding.
As innovations like machine learning analytics, biosensor tracking, and VR simulation integrate further with evidence-based clinical care, technology will likely play an even greater role in the future of addiction interventions.
Final Thoughts
Technology can help expand addiction treatment access and enhance patient experiences. Online tools aid more people remotely while analytics uncover new insights from data. This offers hope against an urgent health crisis impacting countless lives.
However, innovations may take time to process evidence in some cases. Without ethical grounding and scientific proof, cutting-edge tools lose their meaning.
Technology must serve people—not the reverse. It will always require skilled, compassionate human guidance. Digital engagement complements, not replaces, the human touch, which remains at the core of healthcare. Despite the wise application of tools, healing and recovery still happen between people.
With patient well-being at the center, the possibilities they bring for revolutionizing addiction treatment access, efficacy, and prediction offer hope in addressing an urgent public health need.